Insights from CHIME Fall Forum Focus Group show common trends
Ask two different CIOs what they’re focused on for 2025, and you might get very different answers. But when we asked in the context of an “EHR-first” approach that many CIOs say they adopt, we uncovered several similarities.
A group of CIOs came to our CHIME Fall Forum focus group specifically focused on maximizing their EHR investments and the rest of their tech stack. They were asked what they loved – and what they didn’t. From academic medical centers to regional health systems to behavioral health, from the Midwest to the coasts, they pinpointed three similar themes. Here’s what they said:
- An EHR-First Approach is Working – Mostly
It’s no secret that Epic is much beloved among its customers, especially CIOs. Several CIOs using Epic said it was a great investment. Epic’s integration and interoperability capabilities in particular got shout-outs:
- An academic medical center loves Epic’s Care Everywhere interoperability to inform care for patients who travel in from around the state.
- Epic’s ability to integrate with payers was cited as a big efficiency improvement.
But Epic wasn’t the only EHR with devoted customer advocates – MEDITECH received high marks for its collaboration and ability to support co-development with its customers.
Investing in the EHR was consistently highlighted as a priority, with the EHR driving many strategic investments and programs. But these pain points were common, even among EHR advocates:
- Training and maintenance are a challenge.
- Problem-solving and solutions that have worked for others could be more broadly shared among fellow EHR customers.
- It can be difficult to understand how changes to the EHR might affect other decisions or workflows later on.
- The Brightest Spots: Co-Creating Clinical Innovations
Focus group attendees often called out clinical workflow improvements co-created with their EHR vendor as a source of pride. Examples included:
- Using genomic data in MEDITECH for precision medicine.
- Adoption of the Epic physician builder framework, in some cases with 20+ physician builders at an organization.
- An updated care team-to-clinician calling workflow.
However, these workflows might not be perceived as bright spots for the EHR vendor as much as organizational points of pride. Several attendees called out their organization’s own reputation for high-quality clinical care as a driving factor in their technology strategy, and many of the same clinical workflows that were highlighted as co-innovations came with their own EHR challenges like speed of deployment.
- No-Shows Remain a Persistent Challenge
When asked what they’d most like to change, or what would be their top priority for improvement, the leaders were unanimous. No-shows and related schedule utilization challenges, like filling the open slots and getting patients who missed appointments back on the schedule, were the top answer across the board.
Even CIOs at organizations with robust EHR tools for schedule management and patient self-service called out no-shows as the biggest challenge that technology could solve. Some highlighted the significant revenue losses when slots aren’t filled or the heavy staff lift to fill last-minute openings.
The no-show challenge fit into the larger theme of CIOs’ EHR wish lists: they wanted less maintenance, less manual work, and less starting from scratch to solve the same problems as peers – with great results for basic workflows, plus the opportunity to innovate.
—
At the 2024 CHIME Fall Forum, attendees had begun looking ahead. They looked to 2025 and to ways to solve pain points while remaining EHR-first (or, in some cases, switching EHRs to begin building an EHR-first strategy).
For the most part, they felt they were on the right track. An EHR-first strategy unified the technology stack, enabled innovation, and facilitated core workflows well for the majority of attendees. Efficiency was the main pain point, with maintenance, training, and support coming up frequently. No-shows united the entire group as a common and persistent challenge.
Based on the feedback, in 2025, we can expect to see leaders like these focusing on efficiency. Innovative clinical care is a bright spot, but enterprise-wide efficiency and access will likely drive strategy.
This article was originally published in Becker’s Hospital Review.
Across the health IT industry, leaders are balancing pressing concerns like increasing call volume and the need to maximize revenue with limited resources. And nice-to-have initiatives just don’t cut it anymore, with those that don’t drive revenue left on the cutting room floor. So how do you balance building for the long term with the pressures you’re managing right now?
In the webcast Digital Health: On Air, leaders in a variety of roles have shared the challenges they’re facing – and the strategies they use to achieve success in spite of them. Here are some of their takeaways:
Take an incremental approach
In healthcare, “change can be very, very challenging,” says Arz Raheem, Sr. Director of Digital Transformation at Montefiore Health System. “[But] I think, after many years, healthcare is open to the change that is needed. And even if that’s iterative, that’s fine.”
Investing in a large-scale transformation project might be off the table for your organization right now. That’s okay, according to Raheem and Tarun Kapoor, MD, Chief Digital Transformation Officer at Virtua Health. And it can even be an asset.
“In our hypercompetitive market, speed to impact is worth a lot,” says Kapoor. “And so you have to think about, ‘What is the problem that the consumer is facing in this specific situation? How can I make them successful?’”
At Virtua Health, Kapoor’s iterative approach created real clinical impact. Realizing that some patients weren’t responding to colonoscopy reminder outreach, he took a step back. “Traditionally, we say, ‘you have a care gap. Come into the office so we can talk to you about this care gap.’ Instead, we said, ‘we know you might not have time to come in right now. Can you do a Cologuard® test at home?” After this more tailored outreach to a specific subset of patients, Virtua Health got thousands of home tests back and found nearly 300 patients with positive results.
Instead of taking months to work toward a larger project and hit a number of defined milestones, Raheem says, he’s also seen results from an agile approach where projects are smaller-scale and can be expanded later, if they’re successful. An important caveat: “Be brave enough to kill it if there’s no value.”
Bring varied stakeholders to the table
So, what’s the most important ingredient in this iterative approach?
“We try and find people from operations; finance; security; compliance and legal; who are open to change, who can be our champions,” says Raheem. “[Then] we can take good ideas from ideation to implementation and make sure that we’re creating value,” he says.
Gathering this multi-stakeholder group and approaching challenges from this lens requires a culture shift, says Raheem, from the traditional health IT implementation model.
“Technology has had, in my opinion, a culture of more preservation and maintenance. I say, ‘I’m going to try small things. I think I’m onto something and want to show you what I’ve got.’ But if you don’t have the right support, great ideas will die on the vine.”
At the same time, this “coalition of the willing” across different areas of expertise is especially important for Raheem, who serves one of the country’s leading academic medical centers, to avoid introducing risk with an agile approach.
“We’re agile, but we have to be extremely careful about how we implement change and how we’re introducing new technologies because we’re in an environment that is heavily regulated,” he says. So, “if you don’t have that support, then speed to impact doesn’t really happen.”
Pinpoint your pain points
Another way to create outsize success? Pinpoint very specific use cases for new technology, like Main Line Health.
First, Main Line Health identified that their call volume was too high for staff to handle. Having already successfully transitioned to a centralized call center and offloaded some calls to an external resource, they needed another lever to help patients get to the right place without waiting on hold.
Next, they identified that a majority of incoming calls were to schedule mammograms and DEXA scans. “The largest service line supported by central scheduling is radiology and imaging,” said Noreen Friel, Director of Call Center Operations. “And we’ve been trying to increase access to our digital front door and enable patients to schedule themselves.” With a defined scope of the types of calls they wanted to assist with self-service, they were able to quickly add a call-to-self service workflow for patients that would allow scheduling for mammograms and DEXA scans by SMS if the patient desired.
Since adding in the self-service option for these types of calls, Main Line Health has saved 900+ hours in a single year while still getting patients what they need. Pointing to the success of the project, Friel says: “We already had self-scheduling, and we kept it pretty simple. So it was implemented very fast.”
Look for hidden barriers
As your health system is evaluating what’s necessary for the short-term and where to focus for the long term, Elizabeth Woodcock, DrPH, MBA, FACMPE, CPC, founder and executive director of the Patient Access Collaborative, encourages looking for hidden access barriers.
Hidden barriers, says Woodcock, exist throughout the patient experience and can often be resolved to create more equitable and smooth access to care. These barriers could include:
- All patient outreach in English, at an organization where 20% of patients speak Spanish
- Confusing parking or lack of directions to the right office at a large health system
- Required information, such as address, that prevents patients without that information from completing new patient intake
- Lack of accommodations such as free parking for patients who can’t afford a parking deck fee
Better patient access or transformation of the experience doesn’t have to be out of reach if your health system is focused on containing costs through this year and next. Consider low-cost changes that could address these hidden barriers, such as:
- Having your call center staff who speak Spanish accessible through a bilingual call center line
- Providing detailed instructions for parking and locating their doctor’s office for patients coming to your facility for the first time
- Making address or phone number fields optional on electronic new patient forms
- Asking patients if there are accommodations that would make getting in the door for their visits more accessible
Woodcock says that the number one best tool leaders can have for transforming patient access is to “really, really listen.” And as part of this listening, understand that finding hidden barriers requires more creative thinking than simply consulting patient feedback surveys, as these are often a “biased sample” of only patients who have been reached in the right way and in the right language, Woodcock says.
Ultimately, Woodcock points out, searching for and addressing hidden barriers is worth it. “Our most vulnerable patients’ voices are not being heard. And because of that, they’re fighting to get in our system.”
Take a look at cybersecurity basics
The rising threat of cyberattacks means it’s impossible to focus on iterative, impactful changes without a strong security infrastructure. And the very digital transformation that helps create these changes creates more risk, according to security expert Brent Williams.
“Healthcare is a target-rich environment,” he says. “Think about the datasets that are out there – it’s really powerful in terms of stealing identities. In the last 10 years, malicious actors have definitely noticed that, as the digital aspect of the healthcare business continues to grow.”
A core component of a secure health system, according to Williams, is a company culture of security. “The term I use is ‘business as usual.’ Security, when it’s done well, should just be part of the fabric of your processes, your technology, your business,” he says. To enable this culture, he recommends:
- Making secure processes as low-friction as possible so they’re followed consistently.
- Regular staff education
- Ensuring that everyone knows about your information security and compliance team and brings them in for new vendor evaluations or new hardware
“It’s the same weaknesses over and over,” like unprotected VPN endpoints or login pages, that lead to significant cyberattacks, says Williams. “So I keep coming back to the basics.” And over time, Williams says, “the team starts to get a bias toward, ‘oh, this is working well.’”
While the added scrutiny needed for cybersecurity at today’s health systems can be stressful, says Williams, this basic hygiene can protect against costly and disruptive cyberattacks and allow your health system to focus on other impactful initiatives.
Conclusions
The CIO is at the center of a number of challenges, from serving more patients with fewer staff to remaining competitive without overspending on expensive digital tools. But amidst these challenges, you’re still responsible for directing your organization toward long-term success.
The experts featured in season 1 of Digital Health: On Air are creating immediate impact with long-term potential with:
- Iterative change that avoids devoting long-term resources to projects until they’re proven on a small scale.
- Multi-department coalitions to ensure that initiatives have the right context and considerations needed to be successful.
- Technology tweaks targeted at very specific pain points, like individual appointment types that create high call volume.
- Process changes to solve hidden barriers that might be preventing access to care, driving up ED utilization, or causing frustration and callbacks.
- Strong security basics to avoid dangerous, time-consuming, and expensive cybersecurity threats.
If you’re interested in topics like these or would like to hear more from these speakers, follow Digital Health: On Air on Spotify or subscribe for a monthly episode digest.
Tarun Kapoor, Senior Vice President and Chief Digital Transformation Officer at Virtua Health, sees patients not just as receivers of care but as active partners in their healthcare journey. To him, true patient empowerment means more than meeting requests—it’s about proactively understanding patient needs.
Traditionally, patients were left on the sidelines, overloaded with information.“The goal is not just a transformative solution, but a mechanism where patients can be empowered,” emphasized Dr. Kapoor. His approach at Virtua Health centers on collaborating with patients as active participants in their care, because engaging patients directly leads to better outcomes for both the patient and the organization.
Empowering patients through consumer choice
“I’ve heard some people say patients are less loyal these days. The way I look at it, you can’t assume people were previously loyal if they didn’t previously have choices,” said Kapoor.
“Today’s patients have choices and they’re exercising those choices, which now makes them consumers. Health systems need to think more like retailers in meeting patient needs with just-in-time information through convenient modalities (like SMS), and that’s where we are having great success with Luma,” said Kapoor.
Empowering patients through personal customization
Through partnering with Luma, the Virtua Health team ensures patients receive tailored, relevant information before appointments. Automated appointment reminders engage patients in a friendly and accessible way, making healthcare feel less intimidating.This personal touch has streamlined visits and empowered patients with important knowledge about their health.
With now a 79.34% appointment confirmation rate, partnering with Luma has changed how Virtua Health optimizes appointments, making patient engagement efficient and impactful.
Empowering patients through larger system change
Dr. Kapoor advocates for patients playing an active and informed role in their care decisions, but the first move must be made by the larger healthcare industry: “Patients will not be able to empower themselves unless we create mechanisms to challenge our current system and ask ourselves, are we creating an ecosystem where patients can be empowered?”
Fostering this kind of active patient participation is not just the future of healthcare – it’s the present, and it’s a journey that Virtua Health, with the help of partners like Luma, is eagerly embracing.
This blog was written based on Tarun Kapoor’s 2023 Lumanate keynote presentation. Watch it here.
Utilizing an enterprise EHR system is like traveling on a cruise ship. You and hundreds of fellow passengers are on the same journey, for better or worse. The ship is designed to keep everyone onboard happy. You know which destinations lie ahead, but the schedule may be impacted due to weather.
But what if you want to stay a little longer in one port? What if you need to hurry up and meet friends at a different destination? What if you’re a little seasick and want to slow down? You’re out of luck. There’s no diverting the cruise ship from its set route, even when passengers aren’t on board.
We often observe this in healthcare. Many complex organizations benefit from the immense scope and scale of an enterprise EHR to care for a broad patient population, but one size does not fit all. Patient experience and engagement varies widely. Healthcare is a competitive market. In many regions, patients have a choice about where to seek care. Without IT tools in place to smooth the patient journey, this looks like:
- Missed opportunities stemming from minimal patient portal adoption
- Lost revenue from no-show rates
- Stretched staff manually handling custom workflows in business line silos
Patients’ unique needs would benefit from speedboat flexibility to react to market conditions as they change. Enter patient engagement platforms: a solution that natively integrates with your EHR can implement new outreach strategies and realize results now.
In competitive marketplaces, this is not a luxury but a necessity. If you don’t have the ability to reach patients now, you risk losing them to a facility that can. How do we know? Because 87% of surveyed healthcare decision-makers agree that ability to compete in a marketplace is a driver for implementing patient engagement solutions (source). Fortunately, you don’t have to lag behind.
Fill the Cracks, Fast
What if your organization could start seeing changes in a matter of weeks?
Most systems are designed to work when everything is going right: when patients are fully engaged with all of their tools. In an enterprise health system, the multitude of available tools can flow through a patient portal for a streamlined patient experience. But data shows that more than half of patients aren’t using patient portals, even after receiving opportunities to register.
A platform approach to patient engagement can integrate into the native EHR and bridge some of the cracks with a medium that everyone uses: SMS text messaging.
Unlike enterprise EHR modules, API-integrated platform solutions can be implemented and launched within 45 days – enabling your organization to not just keep up with the Joneses, but surpass their assets.
Break Free from Boilerplate
Why are 89% of patients between the ages of 17-74 reluctant to use online scheduling options? Reasons include lack of access to internet, lack of awareness that options exist, low computer skills, and resistance to changing habits (source). It can be challenging to change their ways when limited to boilerplate messaging options and a set number of scenarios. To activate these patients and keep them within a healthcare network, organizations must be able to think outside the box – and step outside of boxes, too.
Partnership with a flexible patient success platform keeps patients on that journey. Over 1,000 messaging scenarios, and the ability to develop more, will accommodate your unique organization – and your patients – right from implementation.
Don’t Despair: Automate
When complexity abounds, organizations hesitate to adopt patient engagement technologies because their processes can vary wildly across the system. Specialities following different workflows keeps organizational knowledge siloed and ensures that valuable staff time is required to keep patients in-network. Many are surprised to learn that complexity doesn’t have to be a barrier to modernization. In fact, implementation of a platform is often an opportunity to simplify workflows and identify streamlined ways to automate tired processes. Administrators and staff alike are often pleasantly surprised to learn that people don’t have to manually undertake every step of the scheduling and intake processes.
The perfect mix
Automation is a hot topic right now, but it’s important to deploy a strategy that keeps humans involved when necessary. Sometimes it’s best to simplify the easy stuff and leave the personal touch for when it’s needed most. Main Line Health saved 15,000 minutes of human time per month when they implemented Digital Call Deflection. Inbound calls could be diverted to conversational SMS text messaging, enabling the call center to focus on patient interactions that benefited from a human touch.
What next?
Learn how an out-of-box solution can reach and activate the 40% of patients who aren’t using your organization’s patient portal. Request a demo here.
Patient care extends well beyond the minutes that a clinician and patient pass in an exam room together. The ensuing visit notes are just one piece of the continuum. Healthcare systems have long integrated selections from a smorgasbord of technology tools to document care, optimize practice operations, and integrate patients’ financial journeys…with varying degrees of interoperability and success.
Moving into 2024, healthcare providers report momentum towards consolidating tech stacks, looking to existing solutions for add-on capabilities before evaluating new vendors. Many EHR vendors are expanding beyond their core functionality of care documentation with solutions across the patient care journey. But organizations should tread with care.
Enterprise EHR is not one-size-fits-all
Every organization has unique aspects that influence operation. The gap between patient expectations and system capabilities can be massive, presenting many opportunities for patients to fall into the chasm between.
What’s holding patients back? Research indicates that barriers to self-service include access to the internet, lack of awareness of services, low computer skills, and change in the habit of making appointments over the phone or face-to-face. But even for patients who engage with technology, a challenging process is likely to disenchant and deter. Patients expect a frictionless experience. Anything less will stand between them and a completed appointment. No pressure, right?
The good news is, in a competitive marketplace, healthcare systems have a huge opportunity to deliver a seamless experience to keep patients coming back.
Most systems are designed to work when everything is going right: when patients are fully engaged with all of their tools. But data shows that only about 20-30% of patients make it through a manual scheduling process to a completed appointment. In their wake, they leave the debris of administrative burden, network leakage, missed appointments, and ultimately: lost revenue.
To capture maximum value from an enterprise EHR, you will need supplemental capabilities and patient engagement guardrails designed to keep the other 70 – 80% of patients in network.
10 Ways that Patient Engagement Platforms Support Patient Retention
- End-to-end SMS capabilities: Patient portals can be limiting – many features hide behind walls of clicks and require a patient’s full, unsustained attention. Text message outreach can go beyond directing patients to their portal. Reach more patients by enabling them to make an appointment or complete pre-visit paperwork by way of text messages, start-to-finish.
- Smart Waitlist Management: Automate the patient-cancel-staff-scramble with a graceful pivot to an integrated process, filling newly-emptied appointment slots as they arise via automated text outreach.
- Streamlined Appointment Management: Enable patients to schedule, reschedule, or cancel appointments through the platform, reducing no-shows and optimizing scheduling efficiency.
- Automated Appointment Reminders from a Recognized Phone Number: Text blasts are often ignored or filtered as spam. When patients receive reminders via a trusted organization’s phone number, practices realize improved appointment attendance rates and reduce administrative burdens.
- Secure Communication Channels: Stay HIPAA-compliant. Secure communication between patients and healthcare providers can be integrated within the platform.
- Health Risk Assessments: Administer and analyze health risk assessments through the platform, aiding in early identification of potential health risks and preventive interventions.
- Feedback and Satisfaction Surveys: Collect patient feedback and satisfaction surveys through the platform to gauge the quality of care and identify areas for improvement. Automate post-visit follow-ups and surveys to gather insights into patient experiences and monitor recovery progress.
- Pre-Visit Questionnaires: Collect relevant patient information before visits through digital questionnaires, optimizing visit efficiency and information accuracy.
- Remote Check-Ins: The digital front door is in patients’ fingertips. Conduct virtual check-ins through the platform, allowing healthcare providers to focus on what’s important and keep schedules on pace patient well-being between scheduled appointments.
- Billing and Payment Integration: Streamline billing processes by integrating payment functionalities within the platform, enhancing the financial aspects of healthcare service delivery.
Simple, right?
Having all of these in place is great, but if they don’t integrate deeply with your EHR, your organization won’t reap maximum returns. Overworked staff can’t spend time tracking these things down manually. For true Patient Success, these workflows must be deeply embedded in a native EHR, automating processes with closed-loop referrals and EHR writebacks.
Navigating the happy path in the complex landscape of enterprise EHRs requires a thoughtful approach to patient engagement. By addressing gaps with personalized strategies, proactive waitlist management, and consideration of generational nuances, healthcare providers can guide patients seamlessly through their journey, leading to improved outcomes and increased value from their EHR investments.
RESOURCE: Learn more about how Luma integrates with EHRs like Epic to support patient retention.
With fewer staff and more revenue challenges, healthcare organizations need to quickly reach their patients and keep schedules full.
Integrating Luma with their Epic EHRs helps Luma community members superpower their patient outreach. Using patients’ preferred messaging channels makes outreach more effective, while API-based EHR integration means no double-documentation or manual work.
Here are some ways the Luma community gets more out of their workflows.
With Luma integrated with Epic, Luma community members’ outreach is:
Customized
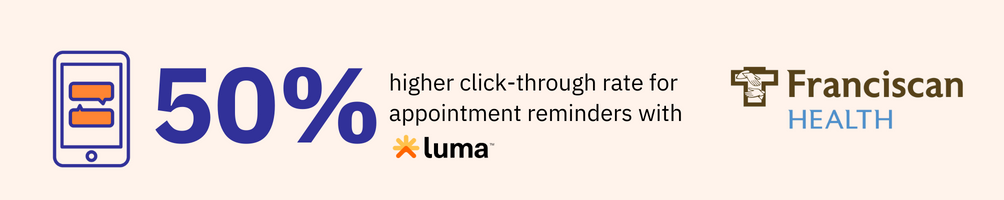
At Franciscan Health, reminders are customized to each patient and appointment type, making them more relevant and actionable.
Details already documented about the patient in Franciscan’s Epic system – from appointment details to preferred contact method – drive the outreach.
For example, patients who have a follow-up appointment the same day or who have previously been seen at Franciscan see different reminders than someone being seen for a new patient appointment.
With these text reminders, Franciscan Health sees a 70% click-through rate – about 50% more than with their previous email reminders.

Text-First
By switching to text-first outreach, Columbus Regional Health immediately saw results. Before implementing Luma, Columbus Regional Health reminded patients about their appointments by automated call, which patients were less likely to pick up or respond to.
“We often have patients make appointments six months out, so it’s important that we provide them with reminders,” said Gayle Wilson, Senior Systems Analyst at CRH.
Luma reminders are automatically sent to patients on CRH’s schedule in Epic. To get even more out of the switch, they made the decision to move from text opt-in to text opt-out, where communication preferences in the EHR use text by default. Now, CRH is sending SMS reminders to more than 80% of their patient population.
Since delivering most reminders via text, CRH has seen no-shows drop by more than 40%.
Actionable
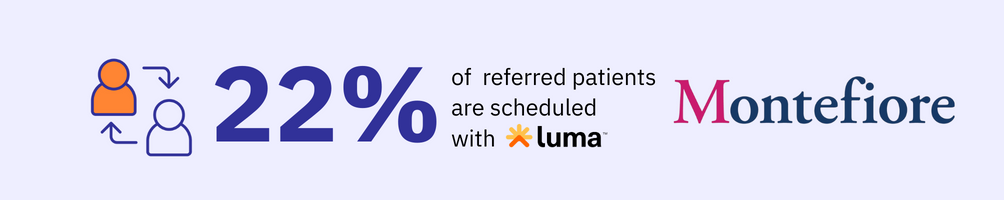
Montefiore Health System in New York sees many of its patients via referral. To ensure as many referred patients get through their doors as possible, Montefiore sends Epic-integrated Luma messages reminding those patients to schedule.
From the message, patients can schedule with just a few taps.
The referral in the EHR is linked to the reminders to keep them up-to-date and actionable. so if a patient hasn’t scheduled, they’ll receive another nudge to schedule. When the patient schedules, the referral is closed automatically and the patient no longer receives reminders.
Want to learn more? Book a quick call with a Luma + Epic expert.
